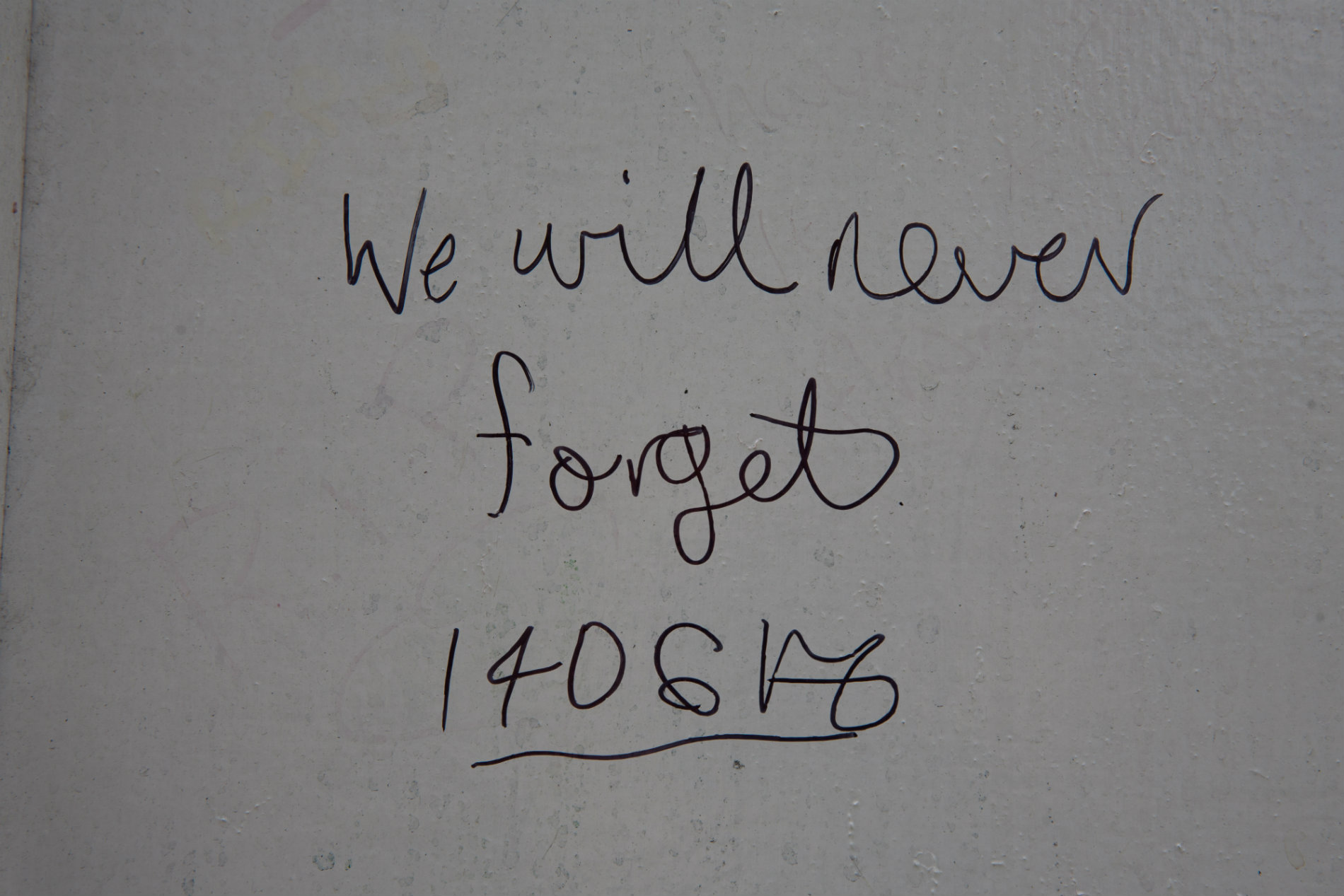
14 June marks 12 months since the fire at Grenfell Tower in London
A tragedy that struck on an unprecedented scale, killing 72 people and affecting many more, the Grenfell Tower fire has had far-reaching effects. Amid the outrage, heartbreak and trauma, nurses have been on the ground trying to bring some hope for recovery to those affected.
One of the first steps taken by Central and North West London NHS Foundation Trust (CNWL) was to put together a nurse-led outreach team. In the immediate aftermath of the fire, initial aims were to offer mental health first aid to survivors, but it wasn’t straightforward.
“Our first barrier was – and still is – engaging people in the community with the idea of treatment. A lot of people don’t want to talk,” says Emma Kennedy, mental health nurse and outreach team manager. “In this situation, there was no model to follow so one of the biggest challenges has been finding creative ways to gain the trust of a distrusting community and working flexibly to respond to needs as they arise and develop.”
Offering services to the bereaved and the survivors was the initial priority and one that was easier to manage. It became more complicated trying to find a way to reach witnesses and other local residents, families and children affected.
We thought we’d be done within a few months but we’ve found that people process at their own pace
The team began by attending community events, wearing green Grenfell hoodies to make their presence and availability known. The response from these identified that there was an immense need for support within the wider population and so they set up a street screening programme, knocking on doors and talking to people.
Trauma symptoms were even more prevalent than anticipated and what quickly became clear was the number and complexity of health needs. It hasn’t simply been a case of treating the ongoing mental health issues that have arisen. As is often the case, the team is also coming across physical health conditions that are inextricably linked with mental health.
“The unique quality of our team, as one comprised of professionals who mostly have training in mental health,” says Emma, “is that we’re able to identify and treat the pre-existing emotional and mental health problems that are often giving rise to further health conditions as well.”
Time challenges of trauma
So far, almost 6,500 people have had contact with the outreach team, with more than two-thirds going on to accept assistance and wider health referrals.
Whereas initially, people were slow to trust and engage, they now seem to be anticipating the arrival of the outreach services with many saying they were simply waiting for the team to come to them.
“We thought we’d be done within a few months but we’ve found that people process at their own pace and you can’t force them to talk about a traumatic experience. We’ve watched, made sure they’re safe, and we’ve waited. Sometimes they trickle in and then there are surges.”

The team is currently made up of mental health nurses, occupational therapists, art therapists, a music and a drama therapist, assistant psychologists and two local residents – one of whom worked in public health and one of whom has a Masters in Islamic studies and spent time in the Calais camps.
Various therapy classes, such as drumming, sculpting and drawing, are put on regularly in community centres and outreach workers are also present to ensure that, should anyone express a desire to talk about their Grenfell experiences, then they are able to get immediate referral to the wider Grenfell team’s therapy services.
Changing the discourse
What has become clear to Emma’s team over the past year is that the needs in the community go beyond the Grenfell repercussions; their work has highlighted how vital and successful a proactive, preventative model of health care can be.
“We have a different approach to other services,” Emma says. “We’re taking health care questions into people’s homes, which is something new. There is a preventative conversation that can be had in their own personal space, giving them the empowerment needed to access health care.”
In North Kensington, around 7% of people suffer with Type 2 diabetes, which only accounts for those receiving treatment and could be significantly higher. This is thought to come down primarily to lifestyle and mental health issues that impede them from pursuing preventative care.
“This isn’t something insurmountable. In fact, we could potentially eradicate this kind of illness and save the NHS a lot of money in the long run,” Emma continues. “Through our work we now have people going to their GPs when they need help instead of feeling alienated by the system. It’s a futuristic model, which certainly needs to be targeted with clear outcomes, but it would be amazing to use this learning as an opportunity to change the discourse in North Kensington and beyond.”
For now, the Grenfell team continues to work tirelessly and, as the one-year mark approaches and the tower is almost fully covered from sight (and set to be demolished by the end of the year), services are expanding rather than slowing down.
Not only do team members aim to provide both mental and physical health care to everyone affected by the fire, they’re also creating an empathetic, humanitarian representation of health care services in which the community can trust.
“That’s really what people want,” Emma concludes. “It’s the way care is delivered that has the greatest impact. Really listening and valuing people, rather than treating them simply as a survivor or ‘the bereaved’, is how we’re trying to make a difference every day.”
Expanding services
The latest addition to the team is Marie Hennessey, a school nurse who will be the first dedicated liaison between the 30 plus schools in the area and the Grenfell team.
“I’ve always had a special interest in emotional wellbeing,” Marie says. “When I saw this post, I knew it would offer the opportunity to really approach school nursing from a fresh perspective. Some of the young people are dealing with extreme trauma and then there are a myriad of other issues related to this. At any time, but especially in these circumstances where people are experiencing issues related to trauma, it’s so important to address health holistically and being part of the wider Grenfell team will give me the opportunity to do this.”
The multi-disciplinary nature of the Grenfell team is what seems to have made it so unique and successful so far. Complementary services working together are better able to create a full treatment pathway and also to benefit from each other’s expertise.
“It’s great to be working with mental health professionals,” says Marie. “They naturally approach things from a slightly different perspective that can be really helpful for me to consider. I suspect they probably think the same about me and my role so it’s beneficial for everyone to be part of this wider team and to tackle health from all sides.”
As a school nurse, you create a link and establish trust with young people and their families
Working alongside both school nurses across the surrounding boroughs as well as with the CAMHS team at Grenfell, Marie will be the joining factor that ensures children are able to access any help and support they might need.
“As a school nurse, you create a link and establish trust with the young people and their families so we’re in the ideal position to act as first point of contact and then refer them on to wider Grenfell team services and beyond.”
This new role is just another way that the Grenfell team is trying to diversify and reach as many people as possible.
“The support is out there,” Marie concludes. “We just want to keep reaching the people that need it and hopefully my role brings us another step closer.”
Seeking support
If you or anyone you know has been affected by the Grenfell Tower fire, visit the Grenfell Health and Wellbeing Service website where you can self-refer for the Grenfell health services.
You can also access a range of support services through the RCN.