Sarah Westcott trains support workers in how to treat pressure ulcers. She shares her expert knowledge on how you can help in the fight against this painful and embarrassing but all too common injury
The cost of treating pressure ulcers in the UK is huge. Treating just one can cost between £1,214 and £14,108*.
The figures are shocking but many of us will have very different concerns. It’s the cost to patients that worries us more. We don’t want to see people in pain, embarrassed, or facing a period of prolonged immobility and an extended hospital stay.
We know that pressure ulcers left untreated can lead to disabilities, amputation, infection, surgery, and can even be life-threatening.
It’s estimated that 50-70% of pressure ulcers are avoidable, but that means knowing what to look out for.
Support workers are on the frontline of patient care so having an understanding of what contributes to pressure ulcer development and prevention strategies is vital.
It's no exaggeration to say you could be a life-saver
Don’t be afraid to ask for training in this area if you haven’t had it. You need to understand the risk factors, what healthy skin is, and the impact of pressure. With this knowledge you can identify and report early signs of tissue damage and take action to help your patients.
It’s no exaggeration to say you could be a life-saver.
*Dealey, Posnett, Walker 2012
The key questions
What’s a pressure ulcer?
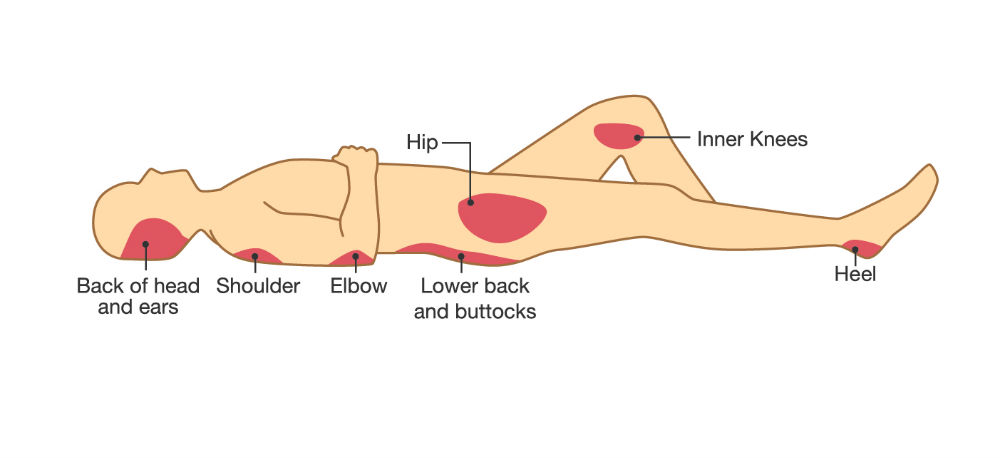
A localised injury to the skin and/or the underlying tissue, usually over a bony area.
What causes a pressure ulcer?
It can be caused by the weight of the body bearing down on a localised area of the skin and underlying tissue. It can also be caused by shear. That’s when part of the body tries to move but the surface of the skin remains fixed.
Can they be avoided?
Absolutely, if the person providing care evaluates the patient’s clinical condition and identifies pressure ulcer risk factors. Interventions need to be planned and implemented in line with recognised standards of practice. They then need to be monitored, evaluated and changed if appropriate.
Some will be unavoidable though, especially if a patient chooses not to follow prevention strategies despite being aware of the risks.
How do you complete a skin inspection?
- Ask the patient to identify areas of discomfort or pain that could be as a result of pressure damage.
- Inspect the skin for pressure damage, including that which may be caused by medical devices.
- Use a validated classification tool to categorise a pressure ulcer. This will guide you on prevention and management.
- Document the results of skin inspections, including detailed descriptions of the site, size and grade. Support this with photographs if possible.

What should you look out for?
Redness to skin, and in darker skin, blue or purple patches; wounds; swelling, shiny or dry areas; hard or warm areas; cold areas compared to the surrounding skin and pain.
What if patients refuse treatment?
The patient’s wishes must be respected. But make sure they’re given enough information to make an informed choice, have capacity to understand the information given, with all questions honestly answered and the risks pointed out. Document everything.
Remember SSKIN
- Surface: make sure your patients have the right support.
- Skin inspection: early inspection means early detection. Show patients and carers what to look for.
- Keep your patients moving.
- Incontinence/moisture: your patients need to be clean and dry.
- Nutrition/hydration: help patients have the right diet and plenty of fluids.
Taken from the NHS Improvement website.
Further information
Sarah Westcott is a registered nurse who runs pressure ulcer training for health care support workers at the RCN in Wales.








