Advanced preparation of insulin syringes for adult patients to administer at home - RCN guidance for nurses
The RCN views the practice of pre-loading insulin as necessary for the small minority of patients unable to use insulin pen devices, and should only be considered after all other options have been exhausted.
There are potential legal and safety complexities associated with the practice of pre-loading insulin syringes in order to enable people to self-administer in their own homes that health care practitioners must be aware of.
Firstly, the preparation of pre-loaded syringes represents a form of secondary dispensing which, under the terms of the Medicines Act (1968), is classified as an unlicensed activity in all four UK countries. Consequently, health care organisations and practitioners must take full responsibility for the safety of this activity.
Secondly, the safety of individuals using preloaded insulin syringes, as well as the storage, stability and sterility of insulin once drawn up in the syringe, is of paramount importance (Rosindale, 2014).
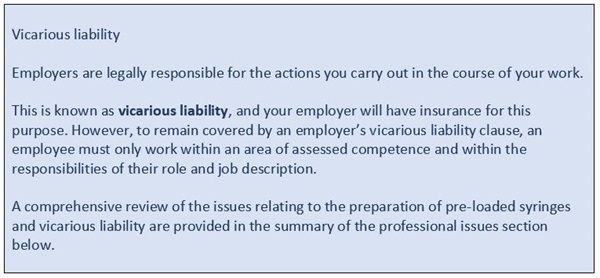
For this reason the RCN recommends that nurses should operate within the framework of a local pre-loaded insulin syringe clinical policy which details the responsibilities of every individual involved in the practice (employing organisation/patient/GP/community nurse) and standardises how nurses perform the preparation of syringes (essential to assure vicarious liability protection for nurses undertaking this practice). Health care organisations and practitioners are also directed to review the Royal Pharmaceutical Society’s Professional Guidance (2018).
An overview of the local framework requirement is outlined in Rosindale (2014) and an example insulin syringe clinical policy document can be found in the appendix on page 29 of this publication.
The policy, which should be regularly updated by a local diabetes lead nurse and the medicines management team, should contain a clearly defined standard operating procedure to guide and support local health care practitioners.
Guidelines
Introduction
This guidance has been updated and replaces previous guidance. Developed for nursing practitioners working in a variety of settings, this publication highlights the professional, organisational and safety issues that must be addressed when pre-loading insulin syringes for later use by a person with diabetes.
Professional consensus statements
Prior to updating these guidelines, the RCN working group undertook an exercise to evaluate the views of senior diabetes nurse specialists and draw on their professional expertise in the development of these recommendations.
The findings of the consensus statement exercise revealed a significant variation of understanding in relation to the professional risks and legal issues surrounding the practice of pre-loading insulin syringes: just 20 per cent of respondents knew the practice of pre-filling an insulin syringe was outside the Medicines Act, and only 20 per cent were aware that pre-loading insulin syringes is not considered to be best practice.
The consensus participants were, however, clearly in agreement on the imperatives relating to patient safety.
They agreed strongly that:
- only registered nurses should be involved in pre-loading insulin syringes
- patients must have capacity for this practice to be considered
- full patient training and education must be provided
- nursing staff cannot undertake this practice if there is no organisational policy in place.
The consensus statement exercise provided the group with an invaluable snapshot of the state of knowledge on this topic, highlighting why the re-issue of this updated guidance is both timely and necessary. The responses revealed how the practice of pre-filling insulin syringes has become so embedded in every day practice that it is often considered normal by many health care organisations and their employees.
It is hoped that these guidelines will prompt a reevaluation and discussion of the issues involved while ensuring that appropriate steps are taken to protect all concerned: patients, nursing staff, and employers.

Context: a growing issue
In recent years the arrival of innovative insulin delivery devices means more people with diabetes have been able to find an insulin pen that suits their needs, reducing the number of people requiring pre-loaded insulin syringes.
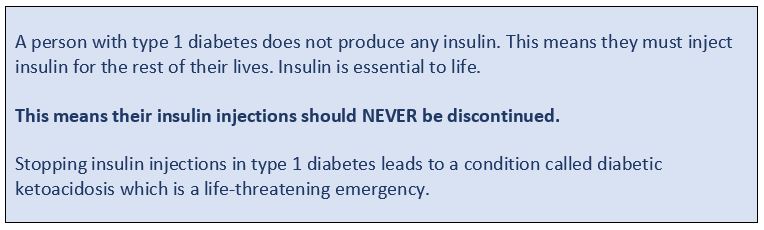
However, there remains a small number of people who will not or cannot use an insulin pen for a variety of reasons: poor manual dexterity; visual impairment; an inability to find a pen device that suits their needs; or a reluctance to make the change from the standard insulin injection syringe they are familiar with (Rosindale, 2014).
As a result, these patients will be unable to autonomously inject once or twice a day and, consequently, will require nursing support to pre-load the insulin syringes they use in order to maintain their independence. The RCN is aware that the potential number of people requiring such support in the community is likely to increase for two reasons:
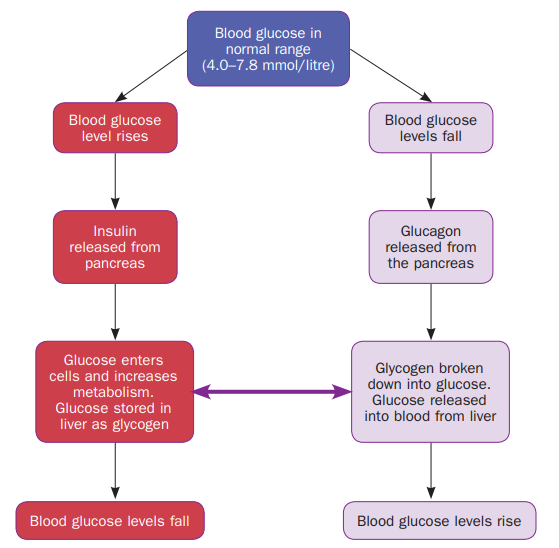
- the number of people with Type 2 diabetes that require insulin treatment is growing: over the past two decades the number of people with diabetes in the UK has more than doubled, from 1.4 million in 1996 to 4.5 million in 2016 (Diabetes UK, 2016)
- Diabetes UK estimates that by 2025, 5.2 million people will have diabetes: most of these cases will be Type 2 diabetes because of the ageing population and the rapidly rising number of overweight people (Diabetes UK, 2016).
The preparation of insulin injections by community nurses for patients to administer in their own homes at a later time has been the practice for many years. Preserving an individual’s convenience and independence, the practice reduces the risk of hypoglycaemia and, by enabling people to administer their insulin at the correct time in relation to meal times, releases nursing time and resources.
Anecdotally, the practice of pre-loading insulin syringes for people with diabetes to administer themselves has taken place satisfactorily for decades. However, there are no national guidelines currently in place to support this practice (Rosindale, 2014).
The RCN believes the practice of pre-loading insulin syringes should only be considered when all other options to enable patients to self-manage have been exhausted – such as the introduction and use of an insulin pen device.
This guidance outlines the key considerations and essential elements that should be in place when the only alternative is to undertake the advanced preparation of insulin syringes for adult patients to administer at home.
Issues relating to prescribing and medicines management are a leading cause of cases being referred to the NMC for consideration of fitness to practise proceedings against nurses and midwives. Following these guidelines should ensure that nurses avoid finding themselves in a position where they are referred to the NMC for inadvertent or deliberate breaches of medicines management standards. These guidelines therefore provide an essential tool for nurses who work in the treatment of adult diabetics.
Summary of professional issues
The act of pre-loading an insulin syringe is considered a form of secondary dispensing which is not covered by the terms of the Medicines Act (1968). In essence, the act of pre-loading an insulin syringe creates an unlicensed product.
This is an important legal consideration that needs to be taken into account by health
care professionals and employers. If something were to go wrong, it is the nurse who
prepares a preloaded insulin syringe outside the bounds of the Medicines Act that would
be liable (Rosindale, 2014).
These points have significant implications for community nurses. While the pre-loading of insulin syringes is considered to be common practice, ultimately, it is the nurse who is professionally accountable for this action.
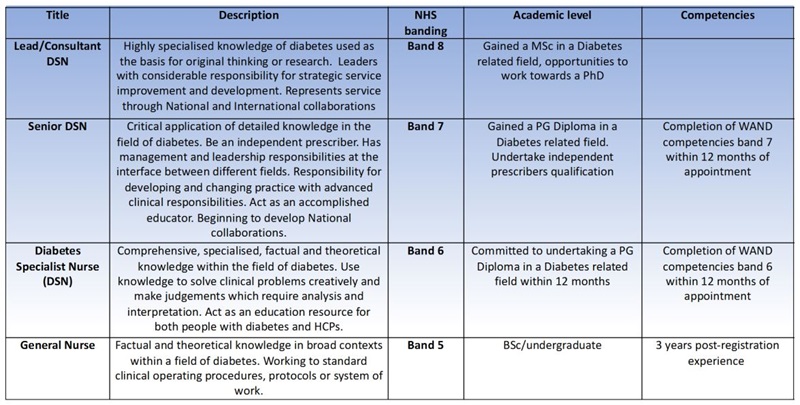
For this reason the RCN recommends that, for their own legal protection, nurses must operate within the requirements of a local policy/protocol for the pre-loading of insulin syringes for patients to administer at home. Therefore, a local policy must be in place to ensure that nurses benefit from vicarious liability, in which the employer takes full responsibility for the safety of this activity.
The pre-loading of insulin syringes should only be undertaken by registered nurses; this
activity cannot be devolved to health care assistants.
Protecting the safety of an individual with diabetes is of paramount importance. In 2010, the National Patient Safety Agency (NPSA) issued two rapid response reports (NPSA, 2010a; NPSA 2010b) highlighting the potential errors that can occur in relation to insulin administration: omitted doses, delayed doses and inappropriate use of non-insulin syringes. However, no harm to patients was reported between 2005 and 2013 as a result of using this method (Rosindale, 2014).
Before preparing to pre-load insulin syringes for adults with diabetes to administer at home, the RCN therefore recommends the following:
Ensuring that there is an organisation-wide policy in place covering the use of pre-loaded insulin syringes; this is essential for your protection and the protection of patients (see Appendix 1 for an example policy document).
- Patients must be assessed and have full capacity for this practice to be considered and patient capacity must be routinely and frequently re-assessed (as per local policy).
- A senior diabetes specialist nurse (SDSN) must be involved in the initial patient assessment; this risk assessment should be updated on a regular basis (as per local policy).
- Comprehensive training on pre-drawn insulin for self-administration must have been undertaken.
- A patient care plan must be in place.
- A quality assurance plan must be in place (as per local policy) which is overseen by your local SDSN.
- The patient’s GP is aware, understands and is in agreement that prescribing pre-loaded insulin syringes has associated medical-legal issues, and that there is a policy in place to support this process.
Patient requirements
A number of essential elements need to be checked when assessing an individual with diabetes who requires pre-loaded insulin syringes. At a minimum the patient must:
- have Level 3 mental capacity, as defined by the Mental Capacity Act (2005)
- accept full responsibility for the storage and administration of the insulin-filled syringes
- be assessed to confirm they cannot use any other first-line licensed alternative (such as an insulin pen device)
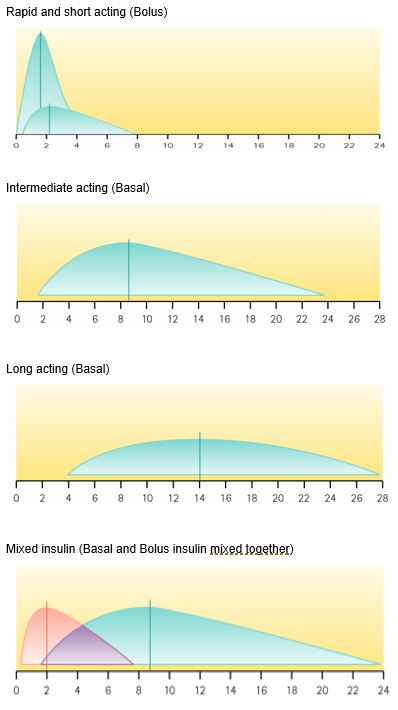
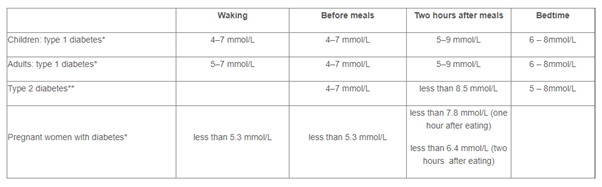
- receive full training and education in their specific medication (dose, frequency of injections, time/action profile), resuspending the pre-loaded syringe, injection technique and rotation of relevant injection sites
- be able to describe the signs, symptoms and treatment of a hypoglycaemic event
- know who to contact should they encounter any problems between visits.
Registered nurse requirements
To benefit from vicarious liability protection, the registered nurse must adhere to the requirements of their local policy for the pre-loading of insulin syringes.
At a minimum, the nurse must:
- always involve the senior diabetes specialist nurse (SDSN) in each patient case
- undertake an initial, and regularly update, a patient risk assessment (as per local policy)
- never delegate the pre-loading of insulin syringes to a health care assistant
- ensure syringes and storage boxes are clearly labelled with content (drug name, dose), time and date of preparation, and patient’s name (as per local policy)
- ensure the patient is educated on their medication, what they are taking and why they are injecting insulin
- ensure patients understand that pre-loaded syringes are their responsibility and are not the responsibility of their carer
- ensure the patient is trained in the correct injection technique (and is still capable of self-injecting), the rotation of sites, the safe storage of insulation and the disposal of sharps
- ensure the patient has a contact number for any problems between visits.
Storage conditions for pre-loaded insulin
In relation to the storage, stability and sterility of pre-loaded insulin syringes in the home, studies have shown these can remain stable and sterile at refrigerator temperatures for up to 28 days (Rosindale, 2014).
Pre-loaded insulin syringes should be stored in the main part of the refrigerator at between 2ºC and 8ºC, and should not be placed in the freezer or at the back of the refrigerator. The needle should point upwards in mixtures containing isophane insulin to prevent blockage by suspended substances in the insulin (Rosindale, 2014).
Lantus (Glargine) or Abasglar (biosimilar Glargine) are unsuitable for use in pre-loaded syringes as it will become turbid (cloudy). Tresiba and Toujeo are also not suitable and should not be drawn from the cartridge or the pre-filled pen into a syringe as it is available in different doses and can overdose the patient.
Syringes should be stored in a sealable container, and both syringes and container should be clearly labelled. If the patient is required to administer insulin more than once per day (for example, prior to eating breakfast, and again, before the evening meal) there should be a separate container for each administration time – even if the doses that are utilised are the same.
Syringe label
The syringe label should contain the following information:
- date and time of preparation
- patient’s name
- name of insulin
- the dose (in number of units)
- the time the insulin injection should be administered
- initials of the registered nurse who prepared the syringe.
Sealable container label
The sealable container label should contain the following information:
- date and time of preparation
- patient’s name and address
- the name of the insulin preparation
- the dose (in number of units)
- administration instructions; for example, just before or 30 minutes before food, at times
- agreed with the patient and documented in the nursing notes
- the number of syringes prepared and left in the container
- the signature of the registered nurse who prepared the syringes.
Separate containers should be used for insulin that is to be delivered at different times of the day.
Whether to re-suspend pre-loaded insulin before injection
If the pre-loaded dose contains isophane insulin or is a cloudy insulin, the syringe should be gently rotated ‘back and forth’ between the hands at least 20 times until the insulin is uniformly suspended before injection. This also warms the insulin, which is important because injecting cold insulin can be painful and is less effectively absorbed.
Potential patient problems
If morning and evening doses are different, it is possible that the two doses may become confused, particularly if the patient has poor vision.
This should be addressed by the community nurse when assessing a patient’s capabilities and circumstances. Ways of overcoming this risk include the use of different shaped boxes for storage, which should be clearly marked to differentiate each dose.
A further potential problem is the accidental wastage of insulin through spillage or the dropping of a syringe, and community nurses should ensure that patients know who to contact if this happens.
Finally, doses could be self-administered at too close or too long an interval. To minimise this risk, the community nurse should regularly assess the patient’s understanding of their regimen and routine.
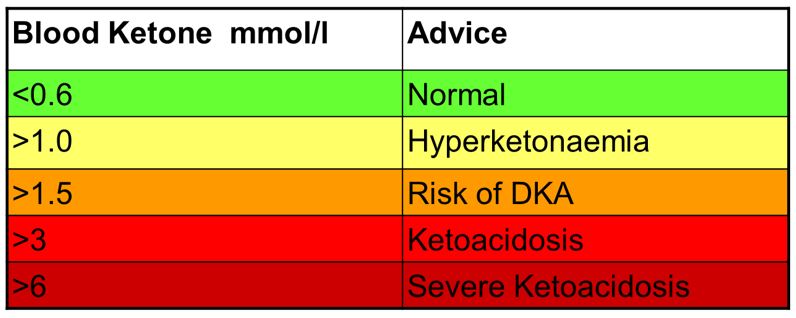
Nursing professionals are responsible for overseeing every aspect of patient safety, which should include the provision of education, support and insulin safety awareness training (including infection control and how to test blood glucose levels).
Disposing of syringes after use
Patients should be provided with yellow sharps boxes to dispose of syringes. These are available on prescription or through the local council, and should be returned in accordance with local guideline on clinical waste management.
Summary of key points
Community nurses are under increased pressure to undertake the pre-loading of insulin syringes for people with diabetes to administer at home.
The rising numbers of people with Type 2 diabetes, combined with an ageing population demographic, means the number of people unable to utilise a pen device due to dexterity or other reasons, is growing. Furthermore, in the current economic climate, there is also a potential for the use of pre-loaded insulin syringes to be abused in an attempt to generate perceived efficiencies by reducing community nurse visits/time.
The RCN considers the pre-loading of insulin syringes not to be best practice, and recommends that the use of licensed first-line injection devices (such as an insulin pen) should be promoted to enable patient self-management.
The RCN advises that:
- the pre-loading of insulin into a syringe for use by the patient at a later date must be seen as the final option, and should only be considered when all other options have been exhausted
- pre-preparing insulin syringes is an unlicensed activity that falls outside the Medicines Act (1968): practitioners and health organisations must take responsibility for the safety of this activity
- an organisation-wide policy/protocol on the pre-loading of insulin syringes for patients must be in place; this is essential to ensure patient safety and provide nurses with legal protection through vicarious liability
- the policy/protocol must set out responsibilities for all parties concerned and set out an agreed standard operating framework for every aspect of the practice (patient education, storage, labelling, monitoring of diabetes control and wellbeing etc)
- the specialist diabetes service/a senior diabetes specialist nurse lead must be involved in the preparation of the organisational policy, the initial patient risk assessment, and ongoing quality assurance to ensure policy adherence.
Consensus statement and methodology
View the Consensus statement and methodology.
References
- Diabetes UK (2016) Annual report 2016
- National Patient Safety Agency (2010a) Rapid response report: reducing harm from omitted and delayed medicines in hospital, London: NPSA.
- National Patient Safety Agency (2010b) Rapid response report: safer administration of insulin, London: NPSA.
- Parliament (1968) Medicines Act 1968, London: Stationery Office.
- Parliament (2005) Mental Capacity Act 2005, London: Stationery Office.
- Rosindale S (2014) Pre-loading of insulin syringes for people with diabetes to administer at home: new solution to an old practice, Diabetes and Primary Care, 16 (3), pp.137-142.
- Royal Pharmaceutical Society (2018) Professional guidance on the safe and secure handling of medicines
Acknowledgements
The RCN would like to thank everyone who contributed to the review and development of this fourth edition.
Samantha Kelly (nee Rosindale), lead author, Diabetes Nurse Consultant for Merton & Wandsworth, Central London Community Healthcare NHS Trust.
Jo Reed, reviewer, Renal Diabetes Specialist Nurse, Imperial College Healthcare NHS Trust
Samantha and Jo were both committee members of the RCN Diabetes Forum at the time of publication.



 Diabetes Research (2021).
Diabetes Research (2021).