Introduction and background

The Career and Education Framework for Cancer Nursing (‘the Framework’) was first published by the Royal College of Nursing (RCN) Cancer and Breast Care Forum, RCN Children and Young People Specialist Care Forum, and the United Kingdom (UK) Oncology Nursing Society (UKONS) in 2017.
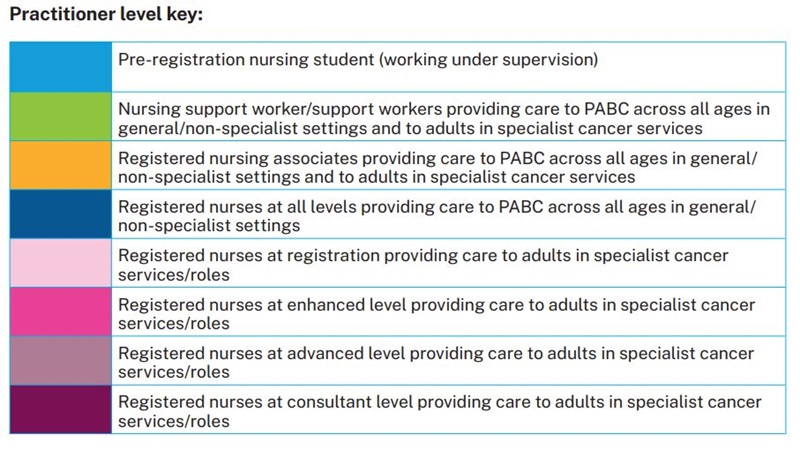
The 2017 Framework for UK nurses was the first to include cancer-specific outcomes for pre-registration students, support workers and registered nurses. This updated Framework incorporates cancer-specific outcomes for pre-registration nursing students, nursing support workers/support workers, registered nursing associates (England only)and registered nurses.
The Framework and cancer-specific outcomes are intended to be used as part of professional, education and workforce development to support improvements in the delivery of high-quality care to people affected by cancer (PABC) by focusing on five workforce groups:
- Pre-registration nursing students to have achieved at the point of registration
- Nursing support/support workers providing care to people affected by cancer across all ages in non-specialist/general settings and to adults in specialist cancer services
- Registered nursing associates providing care to people affected by cancer across all ages in non-specialist/general settings and to adults in specialist cancer services
- Registered nurses providing care to people affected by cancer across all ages in non-specialist/general settings*
- Registered nurses providing care to adults affected by cancer in specialist cancer services*.
The purpose of this publication is to:
- Provide a pathway for career development and a framework for training, continuing development and education for pre-registration nursing students, nursing support workers/ support workers, nursing associates and registered nurses who provide care to adults affected by cancer in specialist cancer services*
- Provide a pathway for career development and a framework for training, continuing development and education for pre-registration students, nursing support workers/support workers, nursing associates and registered nurses who provide care to people affected by cancer (PABC) across all ages in general/non-specialist settings*
- Set out a framework that will help practitioners, employers, commissioners and PABC understand the level of education/capability which correlates to a particular level of practice or role
- Provide information relevant to Higher Education Institutions (HEIs), employers, providers of cancer services, commissioners and policy makers for the development of the workforce, roles, learning opportunities and education programmes
- Provide a point of reference to help identify and develop the knowledge, skills and capabilities in cancer care of the nursing workforce through accredited programmes,and non-accredited learning and workplace-based development opportunities that target not only professional, but local service needs.
* Registered nurses working in paediatric cancer services should follow the ‘Career and Education Framework for CYP cancer nursing’ which is also applicable to children’s nursing students, nursing associates and support workers in paediatric services (forthcoming late spring/early summer 2022).
This updated Career Pathway and Education Framework for Cancer Nursing and the cancer-specific outcomes have been developed and informed by international, European and UK-wide policy for cancer care. These global policies advocate that, for improvements to be achieved in the delivery of care to PABC, workforce development is essential (WHO, 2020). In addition, education standards for pre-registration students (NMC, 2018b) and Registered Nursing Associates (NMC, 2018a), and career pathways, including advanced level practice guidance, are used.
As part of the development and testing of the 2017 Framework and the cancer-specific outcomes, registered nurses providing general and specialist cancer care were involved in the pilot stages. This pilot also included mapping exercises by HEIs against pre-registration and continuing professional development programmes, as well as feedback from an expert group. The feedback confirmed that the Framework and outcomes had the potential to deliver benefits for the nursing workforce, employers and PABC.
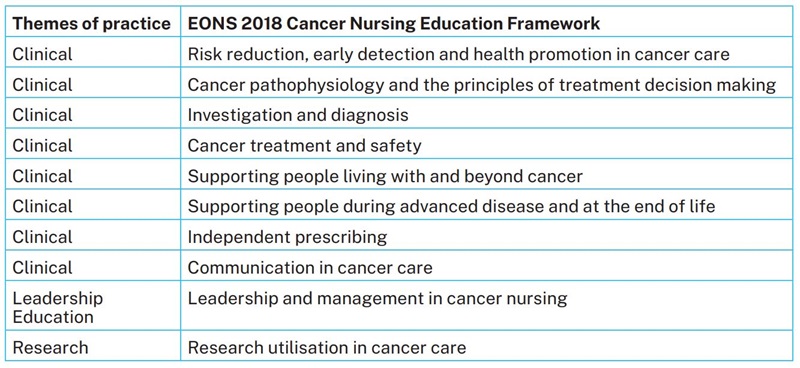
This updated Framework has been developed in consultation with RCN/CCLG Children and Young People Cancer Nurses Community (CYPCN), United Kingdom Oncology Nursing Society (UKONS), the North-west Cancer Alliances (Greater Manchester Cancer Alliance, Cheshire and Merseyside Cancer Alliance, Lancashire and South Cumbria Cancer Alliance) and Skills for Health using the European Oncology Nursing Society (EONS) (2018) Cancer Nursing Education Framework. The outcomes for Registered Nursing Associates have been proposed by UKONS Board members. In addition, as part of the North-west Cancer Alliances and Skills for Health Cancer Nurse Specialist project (Skills for Health, 2021), mapping of the EONS outcomes has been undertaken with their research findings. This mapping confirmed alignment of the EONS outcomes for Cancer Nurse Specialist roles and identified 2 additional outcomes related to ‘investigation and diagnosis skills’ and ‘independent prescribing’. These two areas are included, additional to the outcomes from the EONS (2018) Cancer Nursing Education Framework.
This publication includes:
- a summary of the contemporary UK policy background informing the development of the Framework
- key definitions relating to the delivery of cancer care, levels of nursing practice and pillars of professional practice to structure the cancer- specific outcomes
- cancer-specific outcomes for pre-registration nursing students to deliver care to PABC across all ages in general/non-specialist settings and to adults in specialist cancer services at the point of registration
- cancer-specific outcomes for unregistered nursing support workers/ support workers who contribute to the delivery of care for PABC across all ages in general settings and to adults in specialist cancer services
- cancer-specific outcomes for registered nursing associates who contribute to the delivery of care for PABC across all ages in general settings and to adults in specialist cancer services
- cancer-specific outcomes for registered nurses providing care for PABC across all ages in general settings
- cancer-specific outcomes for registered nurses practising at registration, enhanced, advanced or consultant practitioner levels in specialist cancer services/roles for adults affected by cancer.
The career pathway, cancer-specific outcomes and education framework form a useful toolkit for practitioners, employers, organisations, HEIs, commissioners and policy makers to:
- provide clarity about the cancer-specific outcomes required by practitioners to deliver high quality cancer care and to support their professional development, career progression and professional revalidation
- enable employers and organisations to develop a model for education and training programmes and learning/development opportunities to ensure that the workforce is able to meet the cancer-pecific outcomes to support the delivery of safe and high standards of cancer care
- assist clinical services/organisations with planning current and future services in cancer care, and to provide an insight into the expertise of their workforce
- assist employers and clinical services with designing role descriptors and job plans incorporating cancer care, and to appropriately develop the expertise of their workforce
- assist HEIs providing pre-registration, post- registration continuing development and postgraduate programmes to design and map curricula, and ensure that teaching, learning and assessment strategies help students to develop and demonstrate their knowledge and skills in cancer care within HEI and workplace settings
- enable commissioners to review workplace opportunities, pre-registration, post-registration and postgraduate programmes, and to undertake a gap analysis to commission programmes and learning opportunities that support the achievement of the cancer-specific outcomes required by pre-registration students, nursing support workers/ support workers, nursing associates and registered nurses delivering care for PABC across all ages in general settings and to adults in specialist cancer services
- provide a common language across the UK for role titles, levels of practice, cancer-specific outcomes. This will encourage consistency and sustainability in cancer education and training, and help practitioners demonstrate learning that can be transferred across settings and organisations and inform their career development
- assist commissioners and services to develop minimum standards and key performance indicators for cancer-specific knowledge and skills of the cancer workforce.
Professor Vanessa Taylor, Chair of Steering Group, Deputy Head of School (Students and Teaching), Chair in Learning, Teaching and Professional Practice (Cancer and Palliative Care), University of Central Lancashire.
Cancer is a complex and critical disease that will affect 1 in 2 during their lifetime. The World Health Organization report on cancer (WHO, 2020) identifies that the global burden of cancer will increase with predicted 29.4 million cancer cases/year globally and 1 in 6 deaths due to cancer. In the United Kingdom (UK), the number of people living with a cancer diagnosis is set to double from more than 2 million in 2021 to 4 million in 2030. Cancer is also the most common cause of death in the UK (CRUK, 2021). At the same time, the diagnosis, treatment and management of cancer are becoming more complex with the advancement of scientific and genetic understanding and technological innovations which have the potential to transform our ability to prevent, diagnose, treat and care for PABC of all ages.
It is a common misconception that cancer in children and young people is rare. A child’s cancer risk rises from being very low (1 in 4700) in the first year of life, rising rapidly until 5 years of age (1 in 1000), achieving moderate risk by 15 years, (1 in 450) and a substantial risk by 20 years (1 in 320). These risks are similar to other common childhood conditions such as diabetes, epilepsy and bacterial meningitis, and it is imperative that the whole nursing workforce from pre-registration through to advanced clinical practitioners in primary and secondary care have this awareness (Walker, 2021) There are few clearly evidenced ‘red flag’ symptoms for childhood cancer, although a study by Dommett et al., concluded that three visits with the same symptoms (from a set of 12 common symptoms identified) within three months raised the risk for a cancer diagnosis by ten-fold (Dommett, 2013). Two evidence based public awareness campaigns are trying to influence the public’s perception of childhood cancer, one already published for brain tumours, HeadSmart, and the second, Child Cancer Smart for all other cancers in childhood is in progress (2021). Cancer is also the biggest cause of death by disease in children over one year of age.
Demographic statistics also show increasing numbers of older people in the population. By 2031, 26% of the population will consist of individuals over 65 years, with those over 80 years comprising 8.2%. The ageing population profile points not only to an increasing incidence of cancer in the future, but also to an increase in cancer in individuals who will be living with other chronic conditions.
Never has the time to focus upon the cancer workforce been more critical. This has been emphasised in the implementation plan in Chapter 08, of the WHO report. The report’s recommendations numbers 8 and 9 confirm the need to train and optimise the workforce. The importance of developing the cancer workforce has also been emphasised within Europe and the UK. The European Oncology Nursing Society (EONS, 2018) Cancer Nursing Education Framework, for example, identifies the fundamental knowledge and skills required for post-registration nurses working with PABC. The significant role of the nursing and the allied health professions workforce in supporting people to live well with and beyond cancer has been acknowledged in multiple cancer and workforce policies in the UK (NHS England, 2018; 2019a; 2019b; HEE 2019; Macmillan Cancer Support, 2021) including the NHS Long-Term plan (NHS England, 2019a) which sets out a list of key deliverables and milestones for services caring for PABC. Numerous calls have been made to develop the nursing and AHP cancer workforce through establishing nationally agreed career pathways with associated education and development opportunities (NHS England, 2018; 2019a; 2019b; HEE, 2019; Macmillan Cancer Support, 2021; RCN, 2017) to ensure the right number of cancer nurses and AHPs, and a cancer workforce with the knowledge, skills and capabilities to effectively deliver the care PABC need.
The overall purpose of this Framework is to provide guidance regarding the knowledge, skills and capabilities required by unregistered nursing support workers/ support workers, registered nursing associates, registered nurses who care for PABC of all ages in general settings and those who care for adults in specialist cancer services and roles as part of multi-professional teams across the UK nations. These members of the workforce make a critical contribution to the delivery of cancer care and cancer services across primary, secondary, tertiary and community settings, and in supra-regional centres providing care for patients with rarer cancers, not just for diagnosis and treatment, but as a key part of prehabilitation, rehabilitation, recovery, and living with and beyond cancer (HEE, 2019; Macmillan Cancer Support, 2019; Macmillan Cancer Support, 2018a, 2018b; Andritsch et al., 2017).
This Career Pathway and Education Framework for Cancer Nursing (the ‘Framework’) has been updated by the Royal College of Nursing (RCN) Cancer and Breast Care Forum working in consultation with the RCN/CCLG Children and Young People Cancer Nurses Community (CYPCN), UKONS, North-west Cancer Alliances and Skills for Health in response to changes in the commissioning and delivery of health services, the introduction of the Registered Nursing Associate role (England only), developments in advanced levels of practice and publications from the four UK Departments of Health. These all advocate that, for improvements to be achieved in the delivery of care to PABC, workforce development is required.
The 2017 Framework was the first UK framework to include cancer-specific outcomes for pre- registration students, unregistered support workers, registered nurses providing cancer care in non-specialist/general services and registered nurses at different levels providing cancer care in specialist services/roles. This updated version includes the Registered Nursing Associate role introduced in England.
The Framework aims to enhance the delivery of care for PABC in general/non-specialist and specialist cancer services by focusing on five groups:
- pre-registration nursing students to have achieved at the point of registration
- nursing support/support workers providing care to PABC across all ages in non-specialist/general settings and to adults in specialist cancer services
- registered nursing associates providing care to PABC across all ages in non-specialist/general settings and to adults in specialist cancer services
- registered nurses providing care to PABC across all ages in non-specialist/general settings
- registered nurses at registration, enhanced, advanced and consultant levels providing care to adults affected by cancer in specialist cancer services/roles.
The inclusion of pre-registration nursing students aims to develop a level of knowledge and understanding about cancer, cancer treatment and cancer care for all new registrants at the point of professional registration. The cancer-specific outcomes identified for registered nurses providing care to PABC in general/non-cancer specialist services/roles seek to ensure induction, consolidation and ongoing development of knowledge and skills in cancer care. The level of practice and academic/professional preparation identified for registered nurses providing care to adults in specialist cancer services/roles offers a career pathway with consistency of title, skills, knowledge and preparation across the UK.
As part of the development and testing of the 2017 Framework and the cancer-specific outcomes, registered nurses providing general and specialist cancer care were involved in the pilot stages. This also included mapping exercises by HEIs against pre-registration and continuing professional development programmes, as well as feedback from an expert group. This feedback confirmed that the Framework and outcomes had the potential to deliver benefits for the nursing workforce, employers and PABC. This updated Framework has been developed using evidence gathered through a rapid review of literature and policies, mapping of existing competency and capability frameworks, consultation with RCN/CCLG Children and Young People Cancer Nurses Community (CYPCN); UKONS, mapping by North-west Cancer Alliances and Skills to Health to their research findings and work related to the Cancer Nurse Specialist role. This mapping demonstrated alignment to the European Oncology Nursing Society (EONS) (2018) Education Framework outcomes and identified two additional outcomes focused on ‘Investigation and diagnosis skills’ and ‘Independent prescribing’ which are included in this Framework.
The updated Framework is also aligned to and/or informed by:
- Professional Standards Framework (Royal College of Nursing, 2021b)
- Career Framework for Health (Skills for Health, 2010)
- Enhanced Clinical Practitioner Apprenticeship (Health Education England, 2021)
- Definitions and frameworks for advanced level practice (Health Education and Improvement Wales, 2021; Department of Health Northern Ireland, 2018; HEE, 2017b; NHS Education Scotland, 2021)
- Standards proficiency for registered nurses (Nursing and Midwifery Council (NMC), 2018a)
- Standards of proficiency for registered nursing associates (NMC, 2018b)
- Cancer Nursing Education Framework (European Oncology Nursing Society (EONS), 2018).
The Framework offers a number of potential benefits for nurses, employers, education providers and commissioners and, in response to recommendations made by Lord Willis (2015) and, more recently, Macmillan Cancer Support (2021), by helping to promote a UK-wide career pathway for cancer nursing.





 View the
View the