Health Ability Passport Guidance
A health ability passport is a document that details the reasonable adjustments a staff member with health or disability issues needs at work.
Our guidance suggests a format and process for completing a passport, which hinges on open, supportive discussion between line manager and employee.
This guide is for employees with disabilities, impairments. long term conditions and/or who are neurodiverse who are looking to establish sustainable reasonable adjustments and practical support in the workplace. It is also for their line managers and trade union Reps.
The guide looks at how to have open, honest discussions about disability related needs including those with long term conditions at work – and why this approach is effective.
A health ability passport can also be known as a 'disability passport', 'health passport'. 'adjustments passport' or 'workplace adjustments passport'.
Where health ability passports are adopted by an employer and form part of policy, they are most successful. This is because the passport is recognised across an organisation and that’s when it really comes in to its own.
Many NHS Trusts now have their own passport process and it is important to investigate existing employer provisions.
However, this guide can be used by individuals and their managers to establish reasonable adjustments even if their organisation doesn’t use this approach for everyone.
The guidance and its principles can be used when completing an existing template document, and it can be introduced itself across an organisation using our template document or an alternative that suits the workplace.
The completed document should be considered binding so that employees can see that their input and honesty is valued. It should also build in review dates so that both parties can propose alterations when their needs change. This also includes and review dates needed with a specialist team for monitoring a long-term condition.
However, the most important element of the process is the conversation behind the document. So we've included tips and pointers for both employees and line managers to get the best from their meeting.
Research has shown that reasonable adjustments will fail if they are not accompanied by a supportive, positive attitude from colleagues and managers (Gates, 2000). For the health ability passport meeting to go well, staff must feel able to be open and honest about their health. Similarly, they must be able to play a part in educating their line manager and team mates about their situation as required – They should be able to expect to be treated with dignity and respect, but not expect people to “just know” every aspect of their particular condition or what
will help.
Done right, filling in the passport together is an opportunity to begin or build upon a relationship of mutual trust and respect. It allows the employee to feel valued and gives them a platform to speak frankly about their situation. It allows the line manager a chance to ask questions and gain an understanding of their employee’s impairment in a safe environment for both parties.
In that spirit of transparency, guidance for both individuals and their line managers is included here together.
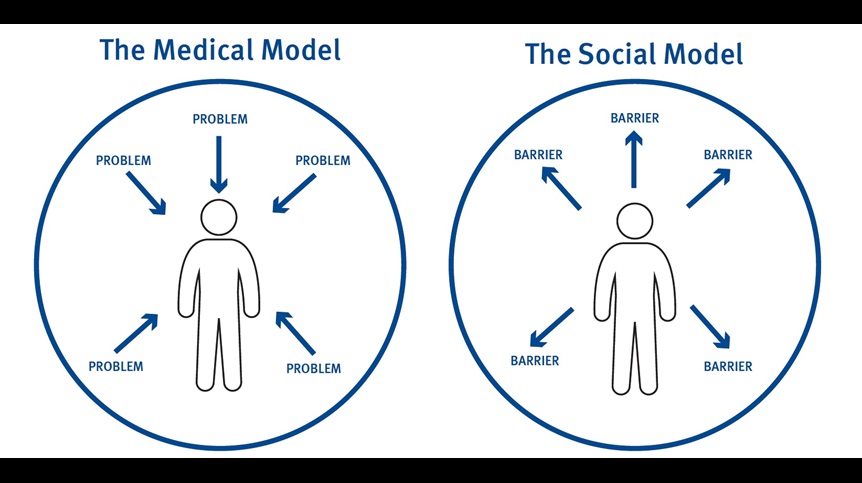
This guidance uses a social model of disability approach.
Under the social model, individuals are disabled by environments and attitudes – not by their health condition or impairment.
This is different to the approach traditionally used in the medical profession, where the individual’s impairment is the root cause of their problems and something to be 'fixed' or 'normalised'.
Whereas some people might say that you “have a disability” under the social model we would say that you “are disabled” – by physical and attitudinal barriers – and the focus is on removing these barriers.
RCN members identify with lots of differing terms when talking about themselves and their impairments. We use 'disability' 'disabled' and 'impairment' amongst others in this guidance.
Everyone will have their own way of referring to their situation and describing exclusion and should be supported to use this. When you're in a one-to-one situation you should use these individual preferences.
This guidance can also be used to establish adjustments if you have a neurodiversity (such as Dyslexia).
A health ability passport can also be known as a 'disability passport', 'health passport'. 'adjustments passport' or 'workplace adjustments passport'.
A health ability passport is a document completed by an employee who requires reasonable adjustments or practical support due to disability/long term condition/neurodivergence and their line manager. It provides a framework within which to discuss the employee’s health and what changes can be made at work to assist them.
Once these adaptations have been agreed the document is signed by both parties to indicate that the adjustments and/or support measures that will be made and upheld. This means that if the employee’s line manager changes they do not have to explain their requirements again and that the current arrangements will not be withdrawn.
Ideally it is recognised within the organisation and can therefore be a valuable resource if employees move to different roles too.
The passport is reviewed at agreed intervals to check that adaptations remain appropriate and can be adjusted if the employee’s needs or their role has changed. Alternatively, to check that the adjustments are still reasonable in line with the employer’s requirements and effective in enabling the employee to fulfil their role. It is a tool to begin conversations about disability/long term conditions and check that the support available is being accessed for example, and Occupational Health referral.
The passport could also be used to discuss and document:
- Who will take which actions, and by when, in order to establish adjustments (eg. contacting Access to Work, procuring equipment)
- A procedure for if the employee becomes unwell, particularly in the case of mental ill health, including who to contact
- Behaviours to look out for that may indicate that health is declining, an episode of illness is beginning
- Things that can trigger or exacerbate the disability or condition and how these can be minimised
- Recommendations from occupational health (if applicable)
- Requirements needed in order to maintain good health eg. Having appropriate reviews with specialists when required
- Related workplace policies eg. sickness absence, disability leave can also be clarified.
For the health ability passport to be effective, it’s important that we understand the value of supporting disabled staff and those with a long-term health condition or neurodivergence.
The RCN has produced this guidance because we appreciate the benefits of a diverse healthcare workforce that includes staff with ill health and disability issues and those who are neurodiverse.
A health ability passport can help retain the skills and experience of staff, many of whom will have gained additional skills because of their own health journey including:
- Increased resourcefulness
- Increased Empathy
- Appreciation of the patient experience
- Determination
Spending some time getting things right at the beginning can pay dividends and bring additional benefits such as clarity when workforce planning.
It’s not only “the right thing to do”; employing staff with impairments, long-term conditions and those who are neurodivergent enriches the workforce, is a positive for patients and is good business sense.
Our leaflet Removing Disabling Barriers at Work explores this further.
The Equality Act 2010 is the legislation in England, Wales and Scotland that details employer’s duties to make “reasonable adjustments” for people who are disabled. In Northern Ireland the equivalent legislation is the Disability Discrimination Act 1995. In both pieces of legislations, someone is disabled when they have a physical or mental impairment that has a ‘substantial’ and ‘long-term’ negative effect on their ability to do normal daily activities – this is a legal, rather than a medical, definition. Anyone meeting this legal definition is entitled to reasonable adjustments by law.
However, at the RCN we suggest considering this as a baseline for determining what support to give staff and ask, if the request is reasonable and will benefit the staff member at work, does the legal definition of disability need to be met?
Tip: under the Equality Act, positive effects of treatment are not considered. For example, someone who suffers chronic pain and meets the criteria of being disabled should still be considered as disabled even if they take medication that greatly alleviates their symptoms.
Reasonable adjustments are anything that removes barriers to allow disabled people the best opportunity to do their jobs. However, when deciding what adjustments you make, as line manager you should objectively consider what is “reasonable” in terms of the role, length of contract, cost of implementation, size and resources of the organisation.
The adjustments themselves are not always physical and can fall in to the following areas:
- Equipment - such as voice activated software, an ergonomic mouse.
- Changes to working patterns - such as shift patterns, working from home, working nearer home.
- Changes to the workplace - such as automatic doors, altered lighting.
- Training - to educate colleagues and change attitudes.
- Redeployment - which means moving to another more suited role that becomes available, when the employee can’t continue in their current role.
- Employer policies & procedures– such as disability leave in addition to sick leave (to avoid triggering sickness reviews due to regular disability related activity such as attending hospital appointments)
The Equality and Human Rights Commission has some helpful examples of adjustments here.
As a line manager, it is advisable to check with HR colleagues when using the passport for the first time to be aware of any wider policies or standard processes related to it.
Employers are legally obligated to provide reasonable adjustments. Refusing to do so or treating an employee differently due to their disability could be discriminatory. The RCN Direct online advice guide Disability Discrimination and the Equality Act 2010 provides further information on this.
Employers do not have to provide an Occupational Health (OH) service to employees. Where they do this could be in-house or provided externally.
NHS Trusts have in-house Occupational Health (OH) provisions for their staff and their role in supporting with reasonable adjustments should form part of employer policy. This would be typical in other large employers too.
If there is uncertainty about OH provision, the HR contact will be able to advise. When OH is not provided via work, an individual's doctor can be involved in discussions.
The role of Occupational Health in this situation is to assess the individual and make recommendations about what reasonable adjustments may be suitable and what work can be undertaken.
In some organisations, a referral to occupational health may be required before reasonable adjustment requests can be considered - in which case a line manager would make the referral. Sometimes an employee can also self-refer. So it’s important for both parties to be aware of any employer policies and adhere to these, and for line managers to know how and when to refer to Occupational Health if requested or indeed required by policy.
The Society of Occupational Medicine (SOM) recommends that where possible a line manager referral is made with agreement of both parties due to the importance of the line manager – employee relationship in the reasonable adjustments process.
Occupational Health services can make an invaluable contribution to the reasonable adjustments process, bringing a wealth of knowledge on what is possible in specific work environments, roles, and for specific conditions or impairments. They should consider the whole person when writing their report; based on time spent with the individual. They believe in the value of work so where appropriate would be looking to support you to remain in employment and equip your manager to best understand your situation and what would help.
The passport document should include a section to detail Occupational Health’s involvement or discuss referring to Occupational Health if this hasn’t happened already.
By agreement it may be beneficial to invite Occupational Health to a “case conference” or consult them during the Health Ability Passport process, if possible.
In the health ability passport there is a section for Occupational Health and specialist team recommendations. Make sure you include the advice of any specialist teams involved in your care (for example a diabetes specialist nurse, or gastroenterology consultant.)
This section can also be used to detail other third party advice from places like the government initiative Access to Work (or Access to Work NI) and specialist charities (for example Action on Hearing Loss for advice on working with a hearing impairment).
If an individual is not confident about what might work, external advice can really help.
There are lots of specialist organisations and charities and a quick web search will be helpful. When reviewing a passport because adjustments are not working or are losing their effectiveness, specialist advice can also really help.
However, many adjustments are simple and it is not always necessary to consult OH (subject to employer policy) or other externals.
By the nature of a condition that is ‘long-term’, it can be defined as a ‘health problem that requires ongoing management over a period of years or decades and is one that cannot currently be cured but can be controlled with the use of medication and/or other therapies’
(NHS Data Model and Dictionary, 2024).
This means that for nursing staff working with a long-term condition, suitable practical support and/or reasonable adjustments may be needed to maintain a healthy work environment.
These requirements for support or adjustments will all be dependent on the individual long-term condition, and advice/support from specialist teams may be needed for line managers to effectively consider how to support nursing staff or students in the workplace. However, line managers should remember that nursing staff may have more than one long-term condition, and each should be reviewed both together and in isolation to ensure appropriate support can be provided.
To ensure safe working in the workplace, only with the individual’s consent, there may be times when sharing relevant information with the wider team is needed to ensure if a problem occurs, an escalation process is in place. For example, there may be a nursing staff member who suffers from epilepsy having a dedicated health ability passport that is shared with the wider team for support on how to manage in times of ill health.
Additionally, to ensure good health is maintained, it is important that those nursing staff members with long-term conditions can attend regular review appointments with their specialist teams. This will help prevent any complications occurring and support good health in the workplace. Line managers need to take this into account when completing a health ability passport with the nursing staff member.
Any RCN member facing issues around nursing with a long-term condition should contact the RCN for support.
Some tips for completing page 1 of the long-term condition passport
If you are using the RCN's template passport document for long-term conditions, it will work best in a PDF reader. You will be able to see tips for filling in the form when you hover over each field. You and your line manager will also be able to digitally sign the document.
- A condition is classed as long-term if there is no known cure and it is lifelong
- Time critical medications are those that must be given at a certain time to support your condition
- Side effects field - List how side effects from medication or treatments may impact on your working day and any related reasonable adjustments needed
- Technology - List any technology and how it needs to be used in your working day. An example may be a blood glucose meter
- Access to private areas - an example may be needing to change a medical device or needing a sterile environment.
Nursing students can use the principles of the guidance to have conversations with their practice supervisor or assessor.
Communication between university and placement provider is often an area of difficulty for students who require reasonable adjustments. Don't assume that because you have disclosed a disability to your university, your placement provider is aware that you require reasonable adjustments.
Be proactive in establishing contact with your next placement as early as possible to discuss your requirements. Check if there is an existing document that you can use to document your requirements, if not a version of our template passport may work for you.
RCN student members who are facing difficulties on placement due to a disability should contact the RCN for support.

Health Ability Passport template
Download our suggested format template which can be filled in digitally or printed.

Long-term conditions passport

Passport to potential
How to complete the health ability passport
Line manager
Send this guidance to the employee and reassure them that your intentions are positive, and that the organisation wants to retain them – this is not a disciplinary or formal capability management process. Invite them to bring notes if they want.
You could say, “I am looking forward to hearing about your situation and working together on your health ability passport. This is not a formal process so there’s no need to worry, but you can
always confirm this by speaking to your union [or failing this a helpline such as Acas] if you want”
Consider if the individual may benefit from being accompanied by a union rep or advocate (most commonly in cases where they are currently off work sick). Alternatively, a friend or family member may be allowed to attend – check your employer’s policy.
Has the employee seen OH? If not and you think it could be beneficial then suggest that you refer them ahead of your meeting.
For those with a long-term condition, have they recently been reviewed by a specialist team? You could suggest they approach this team for advice before proceeding with the passport process.
Set a meeting time that allows a few days for preparation or if applicable enough time to arrange OH or accompaniment.
TIP - Has the employee seen OH? Is a referral to OH an essential first step according to policy at your organisation? If so arrange this ahead of your meeting and await the report before proceeding. Contact the employee ahead of referring to explain the process to them.
TIP : LONG TERM CONDITIONS - for those with long-term health conditions consider if specialist team involvement may be required to help provide recommendations of support/adjustments in the workplace.
Employee
If your line manager has instigated the passport process, this is a good sign. The passport's function is to help keep you in work, so try not to worry.
You can also request the first meeting and share this guidance with your line manager.
Think ahead about what you want to say – make some notes to bring with you if that helps. The next sections of this guide will help you structure your notes. Include positive examples and skills as they occur to you.
If you are off sick at present and completing the DP ahead of your return, then consider if you would feel reassured by attending with a union Rep or advocate. Check your employer’s policy on bringing a rep or friend/family member.
If you need longer to prepare for a meeting, ask to rearrange – but don’t feel that you need to put in hours of preparation. The meeting should be simple and straightforward. If required you can arrange a second meeting.
RCN members should contact us for further advice and support if needed.
Line manager
Whether you know the employee already or not, be clear that this is an opportunity to start from scratch and leave any presumptions at the door.
Explain what the document’s purpose is and that today is about filling it in together. The employee should have seen this guidance already.
You aren’t expected to know all about their condition or impairment - and it can be a hindrance rather than a help to start applying your medical knowledge here.
You are here to understand the employee’s situation and see if together you can reach an agreement that benefits them, your organisation, colleagues and patients.
It should consider any OH recommendations, if an OH assessment has been undertaken. Or any specialist team advice regarding any long-term condition support or adjustments.
Here are some things to cover to make the employee feel reassured:
- Confidentially – where the document will be kept and who can access it.We recommend that a copy is sent to HR and a copy kept by you and the employee.
- Concerns – Make sure the employee has an opportunity to highlight things that may be worrying them about the meeting. They may also worry about wider implications of
completing the passport. Ask, “what would make you feel better about that?” - Own Expert – say something like “I am not here to make assumptions today, I am looking forward to learning from you about how your impairment affects your working life. I may need to ask questions to understand your situation, is that OK?”
- Terms- everyone has different ways of referring to their circumstances. They may or may not consider themselves to be disabled, for example. It is good practice to use their preferred terms. Say something like “when we are talking about your situation, let me know if you have a preferred way of referring to your health issue that I should use.”
We recommend completing the passport together – but you may want to make notes of key things as the employee talks. If so let them know that these are to refer to when you complete the passport.
Don’t forget that any notes you make should be treated as sensitive. Treat them as you would the final document – if you can keep them securely then retaining them with the final document is a good idea. They may be useful if you have to look back at the process at a later date. If you can’t keep them securely, it may be better to destroy them.
Employee
Members often feel very defensive when they have a meeting about their health. It is also natural to look to your manager to have the answers. But this isn’t helpful here.
Remember:
- You have legal rights but more importantly you have valuable skills and experience. You have been invested in by your employer, and it is to their advantage to keep you. Think positive!
- You are your own expert. You probably have coping mechanisms in and out of work already – show your manager how you can meet the duties of your role, have solutions ready. When you don’t have solutions try and work with your manager to work out a plan, consulting third parties if required.
- Leading the conversation. The meeting is focused on your work life but may touch on other areas as it flows. If there is something that you want to keep private or that you are worried will upset you, let you manager know at the outset. You could say “I get quite upset talking about... Can we avoid that please and if it becomes relevant I would rather arrange another meeting so I have time to prepare”.
- Line managers don’t have all the answers! It is so much easier for us to make progress when we speak openly and ask questions. As long as they are asked respectfully, questions from your manager should be seen as a positive - they want to understand and this is better than them assuming. Be prepared to educate your line manager about your condition/impairment if you want to get the best outcome for yourself.
- Don’t be rushed. If you are not sure about an element of the agreement or how the completed document will be used then ask for some time to look over it. Consult your union.
TIP – you should agree who will write up the document. Both parties have time to review it before it is finalised.
Line Manager
Invite the employee to explain in their own words. They should do most of the talking here, you may input to prompt them if they are stuck or to clarify.
Really listen to what they are saying. Active listening means:
- Making eye contact and using body language to let them know you are paying attention
- Having no distractions
- Making only minimal notes
- Allowing natural pauses to occur, without feeling the need to fill the silence
When they conclude, pick up on anything that needs clarifying – things you don’t understand, or elements that are important that haven’t been covered.
TIP: a way of demonstrating that you have heard someone is to repeat back to them. You could say; “you said that you often get headaches after a night shift, how do you manage these?”
Employee
Later on you will discuss solutions with your manager, but this section is really all about you. The notes you have made can help you to give a succinct, structured account.
You could use this as a start point:
- The nature of your health issue including medical name if applicable eg. Fibromyalgia.
- How long you have had this issue if in receipt of a formal diagnosis, when received this.
- What your symptoms are day-to-day. How you manage them.
- If you have a fluctuating condition, how often you have episodes and what, if anything, triggers them.
- Any existing aids or equipment eg. parking near hospital, walking stick.
- How your health issue impacts on your mood.
- Any side effects of treatments.
TIP : LONG TERM CONDITIONS - Provide information regarding your condition, including relevant treatment plans, medications and how your working life is impacted by the condition(s).
Detail any OH recommendations here. If Access to Work (or Access to Work NI), specialist health teams or other third parties such as specialist charities have been consulted then include their suggestions here.
Line manager
At this stage the employee may request an OH assessment – they may not have felt confident to do so earlier. If this happens and you agree this is useful, refer them. The individual may also request they speak to their specialist health team to gain more advice to help complete the passport. Reconvene once the OH report/specialist health team report is received. It will help you both understand the employee's situation and what support and adjustments can help them stay in work.
Employee
If you request an OH report at this stage, keep engaged with the DP process. Be clear that you wish to come back to the process.
If you request to speak to your specialist health team, ensure you are able to get written outcomes of your discussion to bring back to your line manager to complete the passport.
You could say, “Let’s meet again once the report is ready - it will be really helpful to look at it together and work out what adjustments can be made”.
If you are having difficulty identifying the adjustments that would help you, this is the time to adjourn and seek advice. The onus is on you to make contact with Access to Work, specialist health teams or specialist charities.
Write any ideas or suggestions here – both parties can input.
Line manager
Again, this should be offered to the employee to answer first. If they have an OH/specialist health team report they may disagree with this or have additional ideas.
If they seem daunted by the question try and prompt them using your knowledge of what is possible.
Failing this try and find a third party who can assist – a condition specific charity, specialist health team or their union.
See our useful resources and/or internet research. Make sure they leave with a plan of who to contact for advice and document these actions, arrange another meeting so there is a timeline to follow to get information.
Employee
You will probably have some ideas here and should cover as required:
- Shift patterns, change/reduction in hours
- Equipment (don’t forget Access to Work may refund some of the cost to your employer)
- Coaching and coping strategies
- Staff awareness training (this will involve disclosing to your wider team – see step 7)
- Policies and processes that can be changed to support you better.
Additionally, if you have a long-term condition:
- Your review appointments with a specialist team and/or annual reviews that may take place
- Any use of technology needed to support your long-term health condition ie. blood glucose3 meter
- Need for extended rest or break periods to support management of your long-term condition
If at this stage more information is required, make sure you leave the meeting with an agreement on who will do what, by when. This can be recorded in the Actions section.
It is good to include a variety of suggestions, and there is no harm in doing this, but don’t forget that only adjustments that are deemed “reasonable” will be supported.
TIP: Access to Work is a government initiative that can assist with recommendations for reasonable adjustments, and can reimburse employers for part or all of the costs to implement those recommendations. As the employee, you should make first contact with Access to Work. In Northern Ireland contact Access to Work NI.
TIP : LONG TERM CONDITIONS - Describe support that would be reasonable within your workplace and consider any review appointments, use of technology or extended rest/break periods that may be required.
This is where all the discussion so far is boiled down to what is practicable, reasonable in the circumstances and likely to be effective.
The actions may be adjustments themselves, practical support requirements or they may be next steps to take forward as part of the plan such as, researching types of equipment. The could also be agreed processes such as what to do when the individual has a 'flare up' or 'episode'.
The passport can be used as an organic document and signed when both parties are satisfied that adjustments needed are detailed in the actions.
Detail clearly each action and who will do what and by when.
If there is uncertainty about how to take an adjustment or support requirement forward, detail who will look into this and when.
A follow up meeting will probably be needed before the adjustments are in place, to check how things are progressing. Arrange an appointment for this.
TIP: You can’t always be certain that an adjustment will be effective and so you will need to try out some suggestions where practicable to see how they work. There is no harm in doing this, and by building in review dates ensures that where these aren’t effective, other options can be considered.
Use this section to detail what can be shared and who with. If any adjustments or support requirement directly involve the employee’s wider team (eg. staff awareness training) then it will be easiest if they know why.
In general we advise that colleagues know at least some of the reasons for the adjustments. This is for several reasons.
Research shows that adjustments tend to fail when others don’t have a supportive attitude and it is easier to support someone when we know the facts.
If you require any additional support with a long-term condition, it may be paramount that the wider team are aware to ensure you are safe in the workplace. Additionally, through sharing with the wider team they can understand the condition in more detail and begin to understand more about the condition itself.
Disclosure means more employment rights under the Equality Act – if people don’t know, or have reasonable cause to suspect, that you are disabled then they can’t be shown to be discriminatory.
Although disclosing can be scary and feel like an invasion of privacy or an “overshare”, those who disclose often do feel better in the long run as they don’t have to hide who they really are.
To change attitudes in the health care sector, we need colleagues who consider themselves disabled to disclose, so their skills and potential are obvious to everyone.
BUT unless there is potential risk due to the nature of the impairment, choosing to disclose is up to the individual. It may be that once adjustments are made and the process is shown to have value, the employee becomes willing to share more widely.
If the document is handwritten, scan and save it as soon as possible so that it is backed up. Store the original somewhere safely or destroy it.
The document should now be reviewed by the employee and any amendments sent to the line manager for agreement.
Make sure that all adjustments are identified as either temporary or permanent. The document is then signed.
Set a review date. This is a good opportunity to check the progress of implementing adjustments and follow up as required. It is also a chance to assess how effective adjustments are once in place.
If adjustments aren’t working then they can be removed, and other options should be considered.
Make sure it is shared with HR/other departments as required.
Agree a date for review – is there a wider policy around this? We would suggest that this document be reviewed annually at appraisal, and that there is opportunity to raise any issues during other one-to-one meetings between the line manager and employee. It is good to include a caveat around review times so that they can be moved forward if required by either party.
Consider if there is anything coming up that could influence the timeline for review eg. For the employee – an operation; for the organisation – a change to services. If there is, factor that in.
Why is this? Are there legitimate reasons such as difficulty with an equipment supplier or high cost? Or have there been communication issues or a reluctance to deliver? Often this stage occurs because it is not clear who is responsible for implementing which elements of the agreed adjustments.
Revisit your action points. Perhaps it is time for a union representative to assist in negotiations if they haven’t already.
If there is an issue with knowing what adjustments are possible then seek specialist advice – line managers should contact their HR department.
Employers are legally obligated to provide reasonable adjustments. Refusing to do so or treating an employee differently due to their disability could be discriminatory. The RCN Direct online advice guide Disability Discrimination and the Equality Act 2010 provides further information on this.
RCN members should contact us for support and advice.
It is in everyone’s interest to keep a dialogue going and try to resolve issues locally.
Is the reason for the failure obvious? Is it because the agreed adjustments or support measures weren’t working, or because there is a lack of support for them? Are they not sustainable because of other factors such as staff shortages?
If you can, arrange a review of the passport and see what can be updated to make adjustments more likely to work.
Seek outside advice from occupational health, HR, the employee’s trade union, specialist charities related to the employee’s health issue.
If this isn’t possible, or doesn’t work, it is time to find out why and what options remain.
At this stage, if they haven’t already, the employee should seek advice from their trade union or other employment law specialist. The passport document is helpful in evidencing what has and hasn't been done.
RCN members should contact us for support and advice.
Sometimes, despite everyone’s best efforts, it is simply not possible to continue in your current role or to remain in any employment.
If you have explored remaining in work with support to do so from your employer and are satisfied that this is not an achievable outcome, this can be a very difficult time. Health care professionals are rightly proud of the work they do and their caring role forms part of their identity. In addition work is a significant part of our daily lives and losing this can mean losing a lot of social interactions.
You can get past this and the peer support service finds that many people forced to leave their jobs due to health issues do readjust well – it just takes time.
The RCN can offer help:
- Counselling – we speak to hundreds of RCN members every year so we really know the challenges facing healthcare workers.
- Peer Support Service - speak to other RCN members with lived experience of disability issues, so you can get some peer support from someone who knows what it’s like to be where you are.
- Careers - Finding a role that suits your change in ability – look at our careers guidance online, there are some useful tools that look at your expertise and transferable skills. You can also book telephone careers coaching.
- Financial wellbeing - these pages give advice on welfare benefits and income maximisation.
- Regional support – do contact the RCN for support as you negotiate your exit from your employment contract and if appropriate, advice on ill health retirement.
Once you have explored our online resources, contact RCN Direct for referrals as appropriate.
Sometimes leaving your role is essential in order to have time to recuperate and regroup. It doesn't always mean you will never work again.
Ill health retirement needn’t mean you will never work again, but there are a number of criteria to meet and how much you will get is often dependent on your contributions – so make sure you take advice.

Join Peer Support
Page last updated - 11/01/2025







